Benign Prostate Hyperplasia/Enlargement




- Definition
- Distribution
- Determinants (age, race, genetics, lifestyle, and inflammatory cells)
- Microscopic Findings (hyperthropic muscles & inflammatory cells)
- Components (first enlargement & second enlargement)
DEFINITION
Benign Prostatic Hyperplasia / Hypertrophy (BPH) today called as Benign Prostatic Enlargement (BPE) is a non-cancerous growth of the prostate that compresses the urinary tract leading to urinary retention, later bladder outlet obstruction and eventually renal failure. (Figure 1,2,and3)

Figure 1. Normal Prostate |
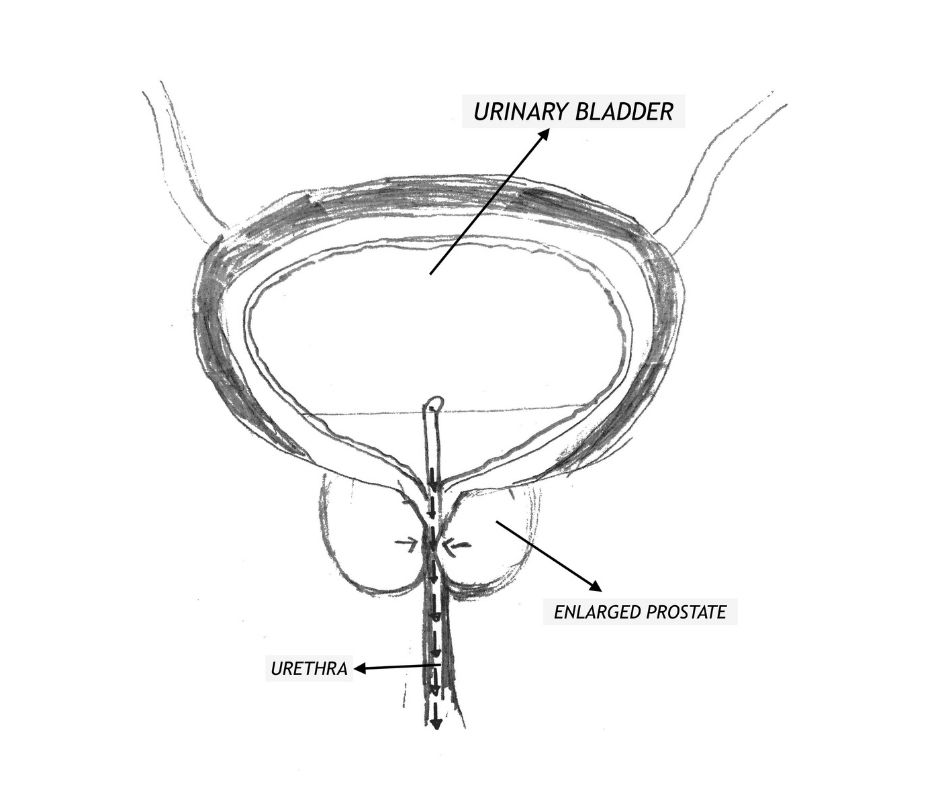
Figure 2. Enlarged Prostate |

Figure 3. Kidney Injury |
DISTRIBUTION
It is a common condition that will affect aging men. 50% of men between 60 and 70 years of age will develop signs and symptoms of prostate enlargement. By age 80 up to 90% will experience a poor quality of life because of this condition.
DETERMINANTS
Race, genetics, lifestyle, age and inflammatory cells are pointed out to be the determinants that influences the development of this disease Race and genetics was argued to be risk factors however epidemiology disproved the presumption. Lifestyle was considered a possible risk factor because many men in the study population were hypertensive and taking beta-blockers, however side effect of the drug has to be considered over lifestyle, besides hypertension has no direct and indirect bearing for BPE. Ageing and inflammatory cells are the most glaring common denominator present in all studies for BPE.
*Aging
Aging is the most constant characteristic feature present in 90% of BPE patients, however, this time element does not explain the condition so that treatment and preventive measures may be formulated. Unlike menopause, that comes surely with age in women, the deficit of female hormones can be measured and when replaced symptoms are minimized. The reverse occurs in BPE, hence cannot be considered as part of andropause syndrome.
*Inflammatory Cells
Lately inflammatory cells have been looked into because of its common findings in biopsied and autopsied specimens. Its presence was only routinely reported sometime in the 90s for lack of awareness. As a matter of fact inflammatory cells are present in all Zones and a consistent findings with BPE and Prostate Cancer (PCa).
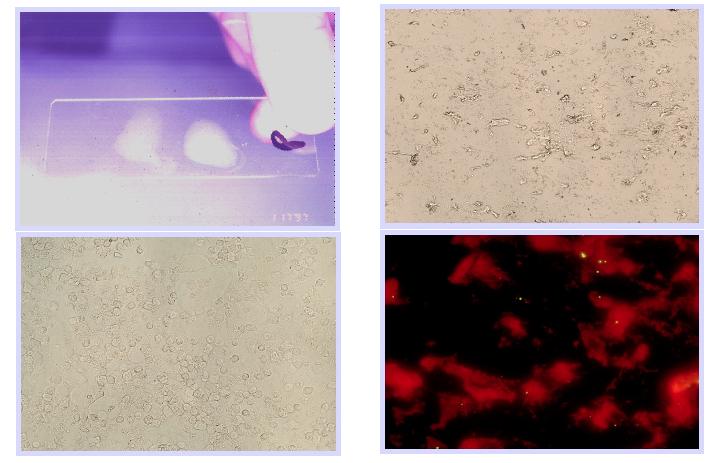
MICROSCOPIC FINDINGS
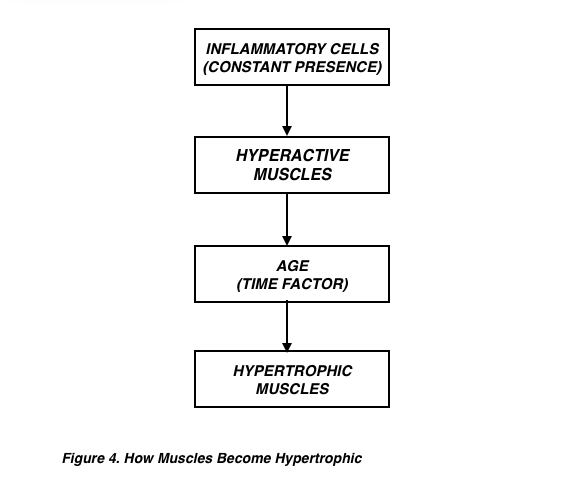
(1) Hypertrophic Muscles
Hypertrophic muscles (muscle enlargement) are end results of frequent muscle contraction. Wear and tear that comes with increasing age and constant presence of inflammatory cells are directly proportional to the frequency of muscle hyperactivity (Figure 4).
(2) Inflammatory Cells
These cells within the glands as seen in expressed prostatic secretions and biopsied specimen causes ballooning of the glands. and consequently increase in size of the entire gland to more than 50 grams.
COMPONENTS
(1) First Enlargement
Purely glandular, ballooning of the glands and can cause the prostate to enlarge even up to 50 grams.
Results of prior TRUS revealed a 92.8-g prostate. Our clinic physician requested that during the patient’s initial visit, Patient 1 take the 5-mg dose of terazosin that he had brought with him. One hour later, the indwelling urinary catheter was removed and prostatic massage was performed. The patient’s prostate was very large and bulged 2 cm into the rectum. The prostate was slightly firm, smooth, and tender to palpation and 4 to 5 drops of EPS were expressed during the massage.
He underwent transrectal ultrasonography (TRUS) of the prostate, which revealed a 27.6-g prostate (a 70% reduction from the pretreatment value).
SEE FULL STUDY: Repetitive Prostatic Massage and Drug Therapy as an Alternative to Transurethral Resection of the Prostate
(2) Second Enlargement
Mostly muscular and sometimes in combination with the First enlargement. Prostate can enlarge to over 700grams.
Table 1 shows the general sign and symptoms of all Prostate Diseases. The predominating presentation of BPE are urinary symptoms. Pain, sexual dysfunction and others can also be present.
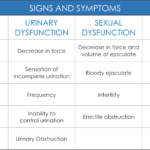
Table 1. Signs and Symptoms
There are two symptoms score questionnaires, the american urological symptoms score and international prostatism symptom score.These questionnaires are use to measures the effects of treatments comparing the before and after symptoms score.
- Patient Profile
- Medical History
- Physical Exam
- Laboratory Findings
- Serology
- Radiology
Patient Type
Symptomatic
- Lower Urinary Tract Symptoms (LUTS)
- Bladder outlet obstruction with urinary catheter
Asymptomatic
- Patients with incidental findings on radiologic and/or PSA
Borrowed Symptoms
- Symptoms picked up from social gatherings with peer group, usual symptoms are Frequency and scanty urination.
Medical History
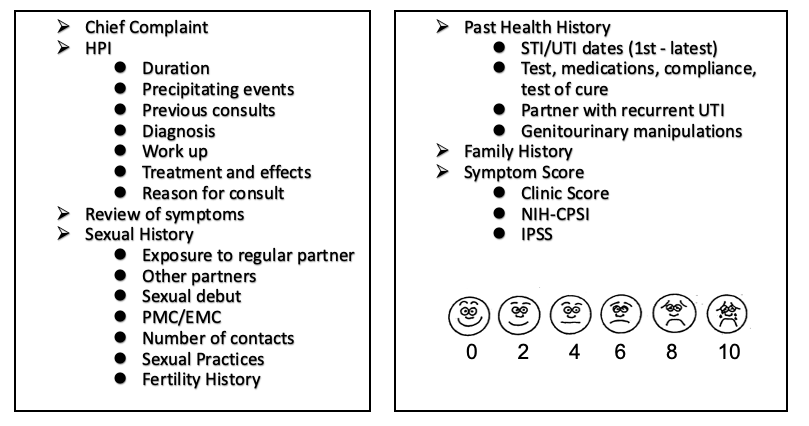
Physical Examination:
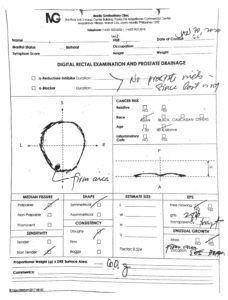
BPE patients will have an enlarged prostate that can be assessed through a Digital Rectal Examination (DRE) and prostatic drainage (See Figure 1).
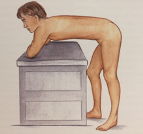
Figure 1. Patient Position |
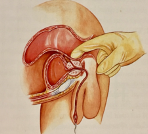 Figure 2. The physician should be able to extract at least four drops of free-flowing prostatic fluid. Figure 2. The physician should be able to extract at least four drops of free-flowing prostatic fluid. |
 Figure 3. Direction of drainage from the lateral to median Figure 3. Direction of drainage from the lateral to median |
Prostate volume can be measured by using the examining finger pulp as a measuring tool. The area of the finger pulp is assigned a value of 10 grams. A normal prostate will have a posterior surface area equivalent to two(2) finger pulps and equaled to 20 grams (Figure 2).
FINGER PULP = 10 GRAMS / POSTERIOR SURFACE
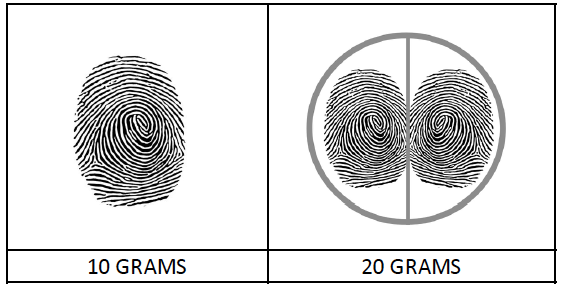
Palpatory findings of the prostate can disclose Six characteristics. These are the following, Median Fissure, Sensitivity, Shape, Consistency, solitary growths and volume as described above. Prostate drainage on the other hand can extract expressed prostatic secretion (EPS). EPS can be give examined both visually and microscopically volume of the secretion can also be measured (see Figure 3). All 6 characteristic findings of the prostate imply the 3 disease of the prostate (Table 1).
The average extraction of a prostate volume of 20 grams is 4 drops. In an enlarge prostate up to 300 drops can be extracted accompanied by a decrease in volume of 40 grams and more.
| FINDINGS | IMPLICATIONS |
| Median Fissure (Palpable, Prominent) | Infection & Cancer |
| Sensitivity | Infection (Acute/Chronic) |
| Shape | Cancer |
| Consistency | Infection / BPE |
| Size & Volume | Infection / BPE |
| Solitary Mass | Cancer |
| EPS (Volume of Fluid & Appearance) | Infection / BPE / Canccer |
Laboratory Findings
Microscopic examination may show excessive WBC and if pathogenic organism are found, patients will benefit with antimicrobial therapy (Figure 5 and 6).
Serology
Prostate specific antigen (PSA) is not recommended for the diagnosis and monitoring of treatment respond for BPE.
Radiology:
Transrectal Ultrasound
This is an ancillary examination that is should be done by a credible radiologist and not by a technician. The examination correlates well with DRE findings for prostate volume. Zonal enlargement (See Zonal Anatomy) is better identified with this procedure and correlates more with symptom scores.
Kidney and Urinary Bladder (KUB)
Measures urine retention and predictive of a pending bladder outlet obstruction.
OBJECTIVES
Prevent the prostate from encroaching the urinary tract.
Non Surgical
- Evacuating excessive trapped prostatic secretion within the glands
- Relaxing the prostate muscles
- Promote shrinkage of the prostate
- Use of devices to drain excess accumulation of urine with in the bladder
Surgical
- Use of dilators
- Scraping of the prostate
- Removal of the entire prostate
- Controlled tissue destruction through heat
THE MANILA PROTOCOL
The Manila Protocol approach in Benign Prostatic Enlargement (BPE) is to remove the accumulated purulent prostatic fluid trapped within the prostatic glands causing glandular enlargement which we call as the first enlargement and to relax the hyperactive prostatic muscle and to control hypertrophy i.e the second enlargement.
SYMPTOMATIC PATIENTS
The first enlargement (see prostatitis treatment). This type of enlargement can cause an increase of prostatic volume to as much as 50 grams. It can also cause bladder outlet obstruction.
The second enlargement is manage by the use of pharmacological agent such as titration of alpha blockers (muscle relaxant) and monitored use of alpha reductase inhibitor (testosterone suppression). Between the first and second enlargement, the former response to treatment favorably on an average of 21 days. The latter takes more time ranging between 4 months to years.
The volume of the prostate is monitored before and after treatment. Residual Urine Volume is also tested to predict & prevent future urinary obstruction.
Treatment Outcome
The application of The Manila Protocol to BPE patients have a variable decrease in prostatic volume to as much as 50 grams and a surprisingly low of 1 gram. Most cases were accomplished within 21 days and many had improvement of symptoms scores. Unexpectedly, we experienced successful removal of urinary catheters to our patient population with bladder outlet obstruction, thus, avoiding the consequences of surgery (See Medical Journal).
FOLEY CATHETER REMOVAL GUIDE (CLINIC’S COPY)
- Pre-Foley Catheter Removal
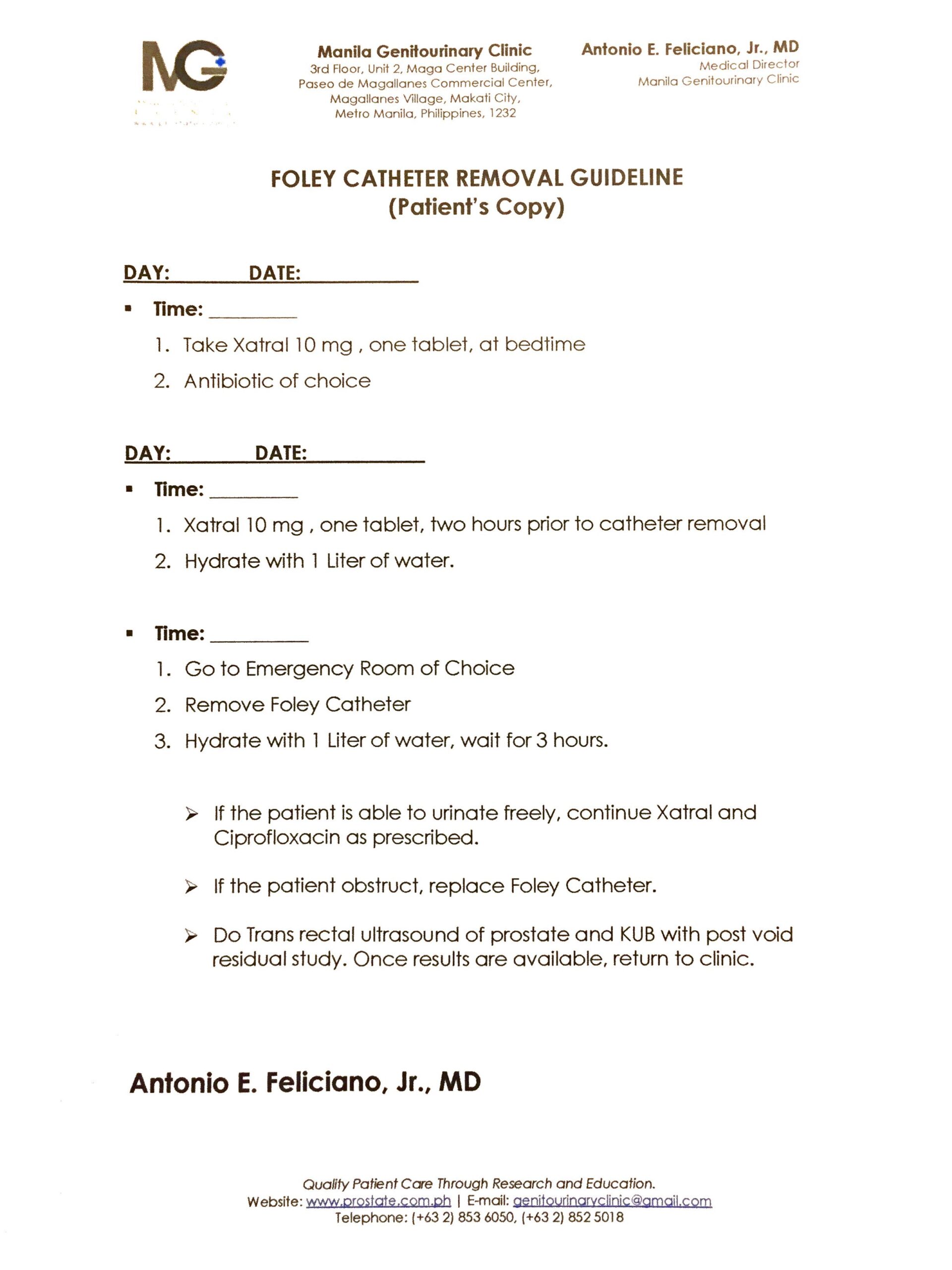
- UTI Documentation and Control
- a-Blocker Loading and Titration (Alfuzosin 10mg OD, 9 hours peak)
- Patient Education on orthostatic Hypotension
- During Foley Catheter Removal
- Time dependent on Peak Plasma Concentration
- a-Blocker Loading (2hours prior to Catheter Removal)
- Actual Removal
- Hydrate with 1 liter of water
- Observe
- Post-Catheter Removal
- If No Obstruction Noted,
- Continue Antibiotic of Choice
- Titrate a-Blocker
- Radiologic Exam
- Prostate size ( Trans rectal Ultrasound)
- KUB with Post void Residual Study
- Return to Clinic for Re-evaluation and Implementation of Manila Protocol.
- If No Obstruction Noted,
Patient with purely muscular enlargement will need maintenance medication. They may encounter manageable bladder outlet obstruction within 3 years.
ASYMPTOMATIC WITH INCIDENTAL FINDINGS
There are patients that consult the clinic because of an incidental abnormal ultrasound and/or abnormal PSA findings. These tests are usually included in a general health check up for males (40 and above) without the benefit of a good patient account of a medical history, clinical evaluation, and physical examination.
It is a common knowledge to doctors that routine radiologic and laboratory examinations lack objectivity. As a matter of fact, most ancillary test have a note below the result stating “THE RESULTS ARE BEST INTERPRETED BY A HEALTH CARE PROFESSIONAL AND ARE NOT INTENDED TO BE USE AS A SOLE MEANS FOR DIAGNOSIS OR MANAGEMENT”. Unfortunately, this is not the case and patients end up with a wrong diagnosis and treatment only to be inconvenience with the side effect of unnecessary medication and herbal supplements.
EXPLANATION TO INCIDENTAL FINDINGS
- Radiology
Generally, suprapubic/abdominal ultrasound of the prostate give a bigger image as compare to a transrectal, hence, a false interpretation of enlargement is not unusual if taken from asymptomatic patient.
- Post void residual urine study: Patients are ask to urinate, an ultrasound of the urinary bladder is taken to identify and measure residual urine. The procedure should be taken immediately after the patients voids. Often times another patient is wrongly put ahead of him, and by the time the delay procedure is done on him, natural urine build up and is measured and mistake for urine retention. As a consequence a normal patients interpreted to have large prostate with some degree of urinary obstruction. These leads to unnecessary medical and even surgical intervention in a normal patients.
- Abnormal PSA findings
Often a routine PSA test is done with justifiable reason and consideration. Recent ejaculation, exercise, intake allopurinol, infection and to mention a few can give elevated PSA values. Goes without saying, iatrogenesis in the making.
It cannot be over emphasize to point out that the patient’s account of a medical history, clinical evaluation with physical examination is extremely important before any investigative study can be order for. The three pillars of diagnosis should always correlated with ancillary examinations. Attending physician should have a direct knowledge or access to the procedure done outside his clinic (see above three bulleted headings).
With a good clinical assessment, together with a dependable and verified ancillary examination the physician can be certain that the gathered data can give him trust worthy interpretation which will lead to a better patient management.
Treatment Outcome
The possible outcomes that result from a thorough evaluation of the incidental findings are: (1) erroneous interpretation of ancillary examination due to lack of good clinical assessments. These patients do not need medications but only realistic patient assurance and the need for a yearly routine prostate examination. (2) those with significant incidental findings are treated accordingly.
See more related Testimonials:
Transrectal Ultrasound-Documented Reduction of Prostate Size
Manila Protocol as an alternative to Surgery
Disappearance of hard nodule-John Garst Testimonials
Previously symptomatic patient with prostate size and volume turned to normal.
- They are seen on a yearly basis for 5 years.
- Symptoms are reviewed
- DRE & EPS are reevaluated
- Radiological studies are compared to results of previous visit.
Patient with maintenance medication
- content
Patient with post-catheter removal
- content