About Urinary & Reproductive System
General
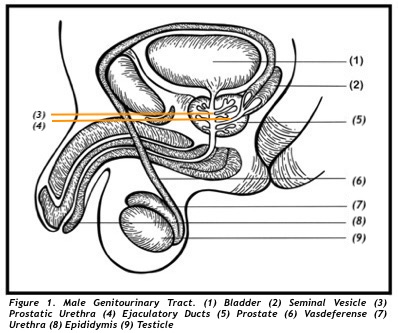
The prostate is network of glands and muscle enclosed in a membrane forming a capsule. It is a part of the male reproductive system. This exocrine gland has a length of 3 cm., a width of 4cm., and a depth of 2cm with a volume of 20 grams. It is located under the urinary bladder (UB) and in front of the paired seminal vesicle. A tube ( posterior urethra) from under the UB penetrates the top of the prostate centrally, and exits at the bottom of the prostate forming the anterior urethra. The urethra drains the UB of urine formed by the kidneys. Two ejaculatory ducts from the seminal vesicle pass through the prostate’s back part and exits the front part, connecting to the posterior urethra (Figure 1). These tubes serves as landmarks for defining the different parts and regions of the prostate.
PARTS AND REGIONS OF THE PROSTATE:
PARTS/LOBES (OLD CLASSIFICATION):
Parts of the prostate are called Lobes and there are four. The anterior lobe is located in front of the urethra. The median lobe is where the two ejaculatory ducts is situated. The lateral lobes have a right and left portion with the tubes at the center. Lastly is the posterior lobe located behind the tubes and is palpable through DRE (Figure 2).
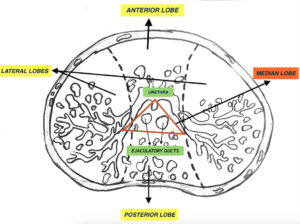
Figure 2. Lobes of the Porstate
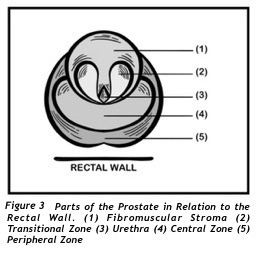
REGIONS/ZONES (NEW CLASSIFICATION):
Regions of the prostate are called Zones. The front part of the prostate is referred to as the Fibromuscular Stoma (Figure 3). Immediately behind this Stroma form the Transitional Zone going backward and curves around the urethra. Behind the urethra and the Transitional Zone forms the Central Zone which cradles the Transitional Zone and the urethra. Last is the Peripheral zone. This zone is located at the back of the prostate and embraces all zones and portions of the Fibromuscular stroma. Zonal and lobular anatomical correlation and pathological significance is illustrated in (Table 1). Zonal anatomy is also useful in predicting the type and degree of symptoms.
| ZONES | DISEASE | LOBES |
| Fibromuscular Stroma | None | Anterior Lobe |
| Transitional Zone (TZ) | Prostatitis, BPH, Cancer | Lateral Lobe |
| Central Zone (CZ) | Prostatitis, BPH, Cancer | Median Lobe |
| Peripheral Zone | Prostatitis & Cancer | Posterior Lobe |
| Table 1. Prostatic Zones | ||
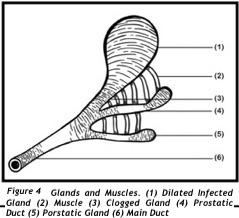
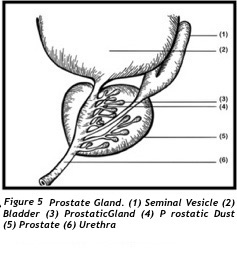
HISTOLOGY (MICROSCOPIC PARTS):
The prostate contains multiple exocrine glands located in all three zones. These individual secretory glands are connected to individual ducts (tubuloalveolar) that branches freely, interwinding with each other repeatedly, and together connects to bigger ducts and ultimately opening to and lining most of the posterior urethra and surrounding the centrally located ejaculatory ducts.(figure 4 and 5).Small muscles envelopes the glands and ducts. Contraction of these muscles expel these secretion to mix with semen during ejaculation.
PHYSIOLOGY (Function of the prostate)
The prostate is a part of the male reproductive system. It`s glands produces a watery fluid secretion. On the other hand prostate capillaries pushes a minimal number of WBC into the glands mixing with the secretion and finally completing the contents of the prostatic fluid (PF).
During ejaculation smooth muscles of the prostate contracts and pushes out the PF to mix with the seminal gel, from the seminal vesicle and sperm from the vas deferens and all together comprises the gelatinous semen later becoming watery.
Prostatic fluid comprises a maximum of 10% (0.5ml) from the total volume of semen around 5ml. Roughly the prostate can produce 10 drops/day of PF which can be described as transparent, colorless watery fluid, containing whitish precipitates (Figure 6).
Figure 6. Sample of Prostatic Fluid
CONTENTS AND FUNCTION OF THE PROSTATIC FLUID (PF):
The PF has two contents. These are secretions from the glands and WBC from the prostate capillaries. Both components, ultimate function, is to help the sperm fertilize the ovum through the following processes. First, release of sperm from the semen (liquefaction).Second provide energy for motility and third is to protect the sperm from opportunistic energy robbing microorganism which interfere with the sperms motility.
PROSTATE SECRETIONS:
Tables 2 and 3 illustrates and outlines the different elements and function of prostatic secretion. To mention a few significant elements are PSA for liquefaction, Glucose provides energy for motility, and Zinc for sperm antisepsis needed outside the male reproductive tract.
Table 2. Prostatic Secretory Products
|
Prostatic Secretory Products |
Actions |
|
Zinc |
Antibacterial Factor |
|
Citrate |
Sperm Transport |
|
Spermine |
Cell Proliferation Odor of Semen |
|
Cholesterol, Lipids |
Sperm Production |
|
Plasminogen Activator |
Semen Liquefaction |
|
Seminin |
Semen Liquefaction |
Table 3. Constituents of Prostatic Fluid
|
Constituents of Prostatic Fluid |
|
|
Polyamines (spermine) |
Prostatic Acid Phosphatase |
|
Plasminogen Activator |
Prostatic-Specific Antigen (PSA) |
|
Seminal Neutral Protease (seminin) |
Electrolytes |
|
Cholesterol, Lipids |
Zinc (prostatic antibacterial factor) |
|
Lactate Dehydrogenase |
Glucose |
White Blood Cells (WBC):
WBC in minimal numbers are constantly present in expressed prostatic secretions (EPS). The WBC increases in number when microorganisms enters the prostate glands. This phenomena protects the sperm while still stored in the vas deference and when it is still being developed in the testicle.
Acid- base balance:
Potential of hydrogen (pH) of the EPS is naturally 6.5 which is slightly acidic. The pH becomes more alkaline during an infection and returns to normal once the infection has been resolved. Perhaps the role of acid-base balance has something to do with antiseptic rather than neutralizing the acidic medium of the vaginal environment as previously thought of.
To summarize it can be hypothesized, based on anatomy, prostatic secretion chemistry and, microscopic study of the fluid that the prostate have four functions. First is for Liquefaction. Second is Energy source for sperm motility and Third is Antiseptic. All three are from the produced by cells of the prostate gland. A fourth function of glandular flushing is recognized by the constant presence of WBC which diffuse into the glands from the capillaries.
Based on secretory components and capillary diffusion
- Liquefaction: Releases the sperm from the seminal gel IE PSA.
- Energy source: Provides fuel foe the sperm’s motility IE glucose
- Antiseptic: Helps prevent microorganism from attacking the sperm IE, zinc
- Glandular Flushing: Removes damaged materials from the glands IE, WBC
PROSTATE PATHOPHYSIOLOGY
FLASHING OF THE GLANDS
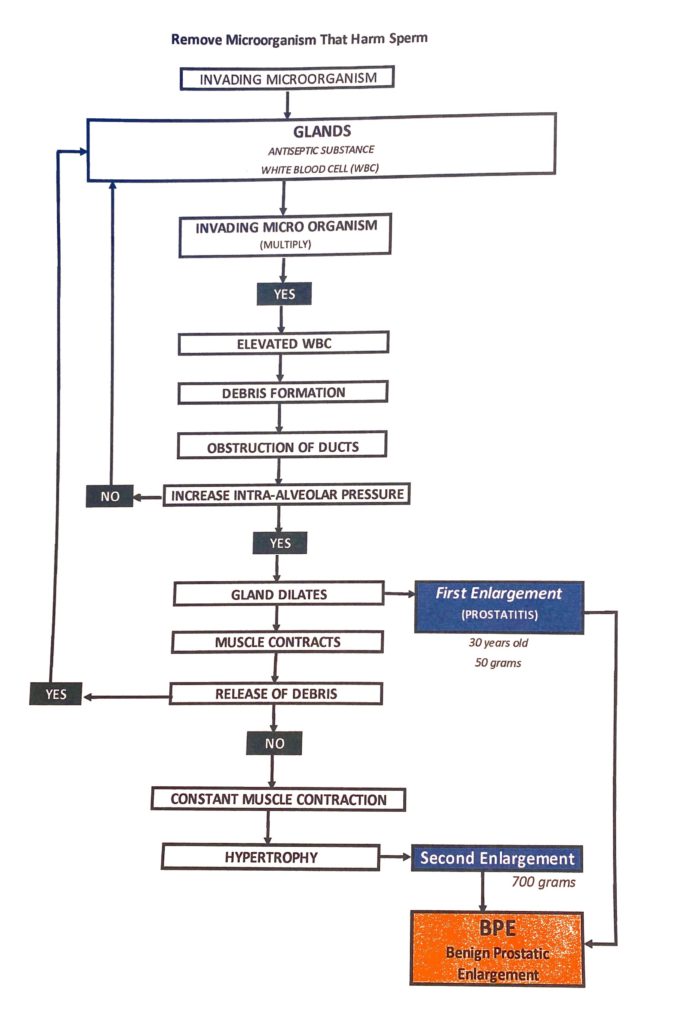
Glandular flushing perhaps will best explain the development of prostate diseases. When invasive microorganism (IMO) enters the glands and all defenses of antisepsis is overloaded with multiplying organism, the minimal number of WBC originally present will start to increase. IMO are destroyed and debris formation occurs within ducts, obstruction of ducts occurs and prostatic fluid is retained within the gland. In effect the volume of prostatic secretion and antiseptic substances are increased. Glands will begin to dilate. Increase intraglandular pressure occurs, smooth muscle contracts, and the end result is waste products are released towards the urethra and eventually outside the body. This process is dynamic and works repetitively in cycles, If this process fails infection occurs (FIRST ENLARGEMENT). Prostate can enlarge to 50 grams due to the accumulation of inflammatory cells alone (See Medical Journal) *Patient1
Flushing of the glands of inflammatory debris require contraction of muscles surrounding the glands and repeated cycles and contraction of muscles always lead to hypertrophy in time (SECOND ENLARGEMENT). This type of enlargement can give rise to a prostate volume of 700 grams, perhaps this would explain why both inflammation and age are the two constant found with BPE (link).