Prostatitis




Prostatitis is commonly regarded as a syndrome (several signs and symptoms with one cause). It is estimated that 25% of men aged 34 will have symptoms referable to the prostate, and by age 40 and above, it is safe to state that 50% will suffer bothersome symptoms related to the gland (sometimes called “headache in the pelvis”). The repercussion of these diseases affects the quality of life similar to individuals suffering from chronic diseases like diabetes mellitus and arthritis.
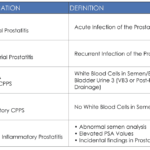
DEFINITIONS & CLASSIFICATIONS:
Technically, Prostatitis means inflammation of the prostate gland. And the most common cause of inflammation is infection, it may be Acute or Chronic. Acute usually have sudden onset and severe symptoms while Chronic have prolonged onset but less severe and persistent symptoms.
Granulomatous Prostatitis in the author’s opinion is a misnomer because of the term Prostatitis. It is neither acute or chronic in terms of inflammatory activity. Perhaps based on pathological, microbiology, physical findings, and anamnesis, and clinical evaluation,It maybe safe to presume that the condition is an after effect of either an infection or scarring due to injury.
There are three medical literature classifications: The 1968 Stamey/Meares Classification, 1990 Manila Protocol and The 1999 NIH Classification.
The 1968 Stamey/Meares Classification
Non-Bacterial and Prostatodynia (Table 1). This classification are symptomatic. The former have objective evidence of inflammation but no documentary evidence of infection. On the other hand, the latter have no objective findings at all.
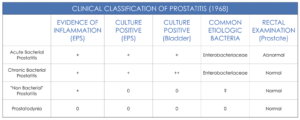
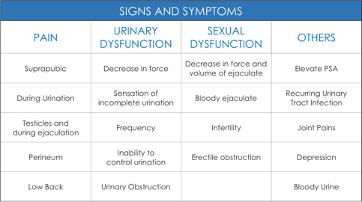
Table 1. Clinical Classification of Prostatitis
1990 to date The Manila Protocol
Define’s Prostatitis as an inflammation of the prostate gland due to infection. It may be bacterial, fungal and parasitic. These conditions can be acute or chronic. The definition is based on the utilization of microbiological techniques in identifying specific organism not seen in the past due to lock of technology.
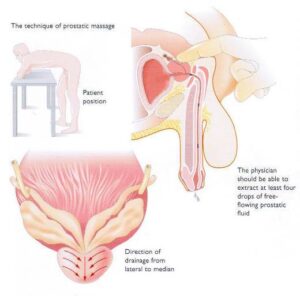
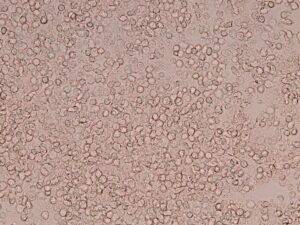
The protocol uses Repetitive Prostatic Drainage (RPD) to expel the inflammatory debris (WBC) and release the hidden organism which can later be identified (Figure 1-(b),(c),(d)).
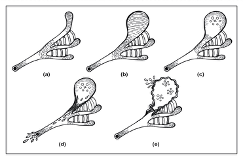
Figure 1. (a) Normal prostate glandular network (b) Glandular swelling (c) Debris formation and clogging of ducts (d) release of obstruction due to pressure increase (e) Mutation and cancer genesis
The extraction of the most purulent Express Prostatic Secretion (EPS) does not occur during the first drainage but on the fourth drainage in most cases. Ducts remain obstructed during the first drainage (Figure 1-b).
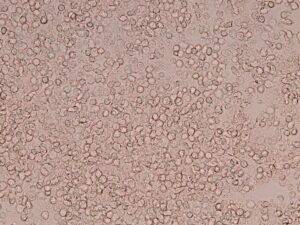
Figure 2. White Blood Cell/OIF Immersion Field. Continuous massages loosen and release inflammatory debris flapped within the occluded ducts. Succeeding drainages reflect the true inflammatory condition of patients with prostatitis
- Prostatodynia (NIH Category III-B)
In most cases drainage 1 shows white blood cell interpreted as normal.
- Bacterial / Non-Bacterial (NIH Category-II /Category-IIIA)
Drainage 2 and 3 shows increasing of white blood cell, compare to drainage 1. Prostatodynia now becomes either Bacterial and Non-Bacterial with the patient.
- Asymptomatic (NIH Category IV)
Drainage 4 and 5 releases the hidden inflammatory cell causing irritation thus symptoms relieved. This is the correct time to extract microbiological specimen.
The 1999 NIH Classification.
Chronic Pelvic Pain Syndrome (CPPS) was later adopted by the US National Institute of Health (NIH) in 1999. There are 4 categories (Table 2):
- Inflammatory CPPS (NIH Category III-A) which coincides with non-bacterial
- Non inflammatory CPPS (NIH Category III-B) coincides with Prostatodynia
- Asymptomatic Inflammatory Prostatitis (NIH Category IV). This findings was also observe in the study of Stamey in 1968 but was never labeled.
Table 2. US National Institute of Health (NIH) Categories
Acute Prostatitis
The onset is usually within several hours. General symptoms are fever and severe pelvic pain described as sharp and burning. Urinary symptoms are severe and there is difficulty in passing urine.
Chronic Prostatitis (CP)
The onset ranges between three months to twenty years. Generally, symptoms are milder but bothersome. Predominating symptoms are pelvic pain while urinary symptoms are less severe compared to the acute counterpart.
Symptomatology (Study of Symptoms) can be subdivided to four groups (See Table 1) Pain symptoms are the predominating symptoms in prostatitis. This is due to the process of inflammation which gradually builds up within the glands level of pain increases (Figure 1). At maximum pressure the toxic substance is released from the glands into the urethra and expelled via urination. Level of pain decreases (Figure 2.D). This will explain the on and off microscopic visualization of white blood cells(WBC) in the urine and semen samples. At the height of symptoms microscopic findings are negligible and vice versa.
TABLE 1
“Medicine a science of uncertainty and an art of probability.”
-Quote by William Osler
General:
Diagnosis of Prostatitis entails scrutinizing and correlating from the patient, information such as Patient Data Base, Medical History, Physical Examination, Laboratory and Radiologic Findings. Prostatitis Symptoms Scores cannot give specific diagnosis. It may be helpful in comparing symptom level before and after treatment. A reliable diagnosis can be attain once bits and pieces of medical information link with one another.
Patient Data Base
To mention a few, comprises of gender (women do not develop prostate diseases). Age, prostatitis is more common in 34 yrs of age, Benign Prostatic Hyperplasia (BPH) usually start at age of 40 and Prostate Cancer typically be detected at age 60. Occupation, profession that requires frequent travels (ex. pilots and engineers) are usually more prone to develop prostatitis.
Medical History
Is similar to a jigsaw puzzle. Bits and pieces of information needs to be connected in its proper order so that the complete picture will be appreciated.
Comprises of chief complain, duration of chief complain, symptoms score, patient reliability, history of present illness, review of symptoms, sexual history and past health history,
- Chief Complain, is the main reason why the patient consulted with physician. It is limited to two signs and symptoms only.
- Duration of Chief Complain, it is the onset of the complain.
- Symptoms Score, is the patients perception of the severity of symptoms.
- Patient Reliability, measures the accuracy of the information extracted from the patient.
- History of Present Illness, describes the sequent of events that lead to appearance of signs and symptoms of the chief complain
- Review of Symptoms, these are other signs and symptoms associated with the chief complain.
- Sexual History, measure the probability in acquiring the disease based on the number of exposure and latest exposure.
- Past Health History, asses if the present condition has been associated with past illness.
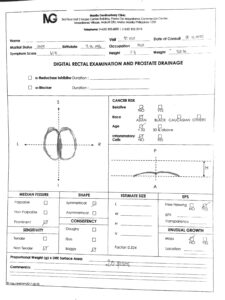
Physical Examination:
Digital Rectal Examination (DRE) is the main stay for detecting prostate diseases. Properly done, a physician may be able to differentiate acute from chronic Prostatitis.
In acute prostatitis, the rectal wall is usually warmth to touch, the median fissure will be prominent, the prostate will be tender, symmetrical in shape and boggy in consistency. EPS is expected to be purulent.
In chronic prostatitis, the median fissure is usually prominent signifying an increase in prostatic secretion trap within the glands. The prostate will not be tender, shape will be symmetrical except in granulomatous prostatitis and consistency usually will be boggy. Transparency of EPS will be found to be from clear to turbid.

Figure 4(a). Express Prostatic Secretion |
Ancillary Examinations
Laboratory and Radiologic Examinations
Laboratory
Includes microscopic and microbiologic,
- Microscopic consist of a wet mount (to mention a few), this examines the EPS. It quantifies white blood cell (WBC) which is directly proportional to the degree of infection. Normal values are between 10-20 per high power field (HPO). Excessive WBC from EPS is specific for Prostatitis.
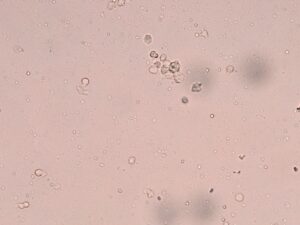
10 WBC
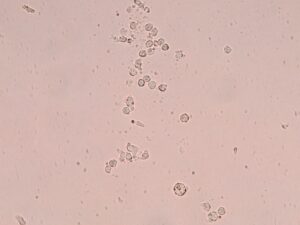
20 WBC
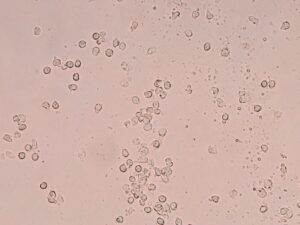
50 WBC
Abundant WBC
- Microbiologic examination is a procedure that identify different organisms using specific techniques such as culture, immunofluorescence and PCR.
- Urinalysis VB 1 (first flow urine) represents the urethra, VB2 (second flow) represents the urinary bladder, and VB3 (urine extracted after prostatic drainage) represents WBC from the prostatic secretion but not as accurate as wet mount taken from the EPS.
- Blood examination examines for Prostate Specific Antigen (PSA). However, PSA should never be use in the screening prostate diseases.
Radiologic Examinations
Ultrasonography and other radiological examination are not useful in diagnosis of prostatitis.
- Treatment depends on the type of infection/s. Target Speicific Antibiotics are given for a minimum of fourteen days, an average of twenty-one days, and no longer than 30 days.
- Antifungals are best given after the course of antibiotics to prevent yeast overgrowth as a secondary infection. Antiprotozoal are also given empirically or specifically.
- Tri-weekly prostate drainage is an important component in the successful treatment especially for chronic prostatitis. It promote defusion of antimicrobials into the gland. It monitors the progress of treatment and it determines when to stop the antimicrobials.
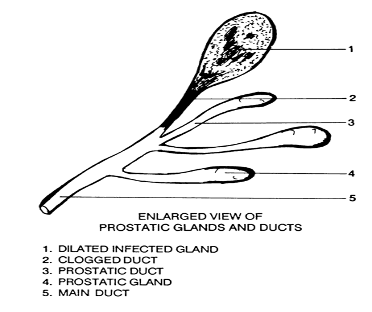 Figure 1. Infected Prostatic Gland Figure 1. Infected Prostatic Gland |
Figure 2. |
 Antimicrobials will not defuse into an infected prostatic gland packed with white blood cell.
Antimicrobials will not defuse into an infected prostatic gland packed with white blood cell.
Drainage flashes out the packed white blood cell from infected gland enabling antimicrobials to freely defuse and eliminate the infection completely.
CRITERIA OF CURE
- Return of EPS WBC count to normal
- EPS, Cleared for GenitoUrinary Pathogens significant decrease of symptoms
- No Recurrences